The exact cause or causes of breast cancer remain unknown. Yet scientists have identified a number of risk factors that increase a person's chance of getting this disease. Certain risk factors, such as age, are beyond our control; whereas others, like drinking habits, can be modified.
The risk of breast cancer increases with age. For example, annual breast cancer rates are 8-fold higher in women who are 50 years old, in comparison with women who are 30. Most breast cancers (about 80%) develop in women over the age of 50. In one age group (40 to 45 years), breast cancer is ranked first among all causes of death in women. Breast cancer is uncommon in women younger than 35, with the exception of those who have a family history of the disease.
If a woman has already had breast cancer, she has a greater chance of developing a new cancer in the other breast. Such a new, or 'second,' cancer arises from a completely different location and should not be confused with a cancer that has recurred (come back) or metastasized (spread) from another site. The likelihood of a new cancer increases by 0.5% to 0.7% each year after the original diagnosis. After 20 years, a woman has a 10% to 15% chance of developing a new breast cancer.
A previous diagnosis of lobular carcinoma in situ (a localized tumor) is associated with a 10% to 30% greater breast cancer risk, and a previous diagnosis of ductal carcinoma in situ is associated with a 30% to 50% greater risk.
Approximately 85% of women with breast cancer do NOT report a history of breast cancer within their families. Of the remaining 15%, about one-third appear to have a genetic abnormality. The risk of breast cancer is about two times higher among women who have a first-degree relative (mother, sister, or daughter) with this disease. The risk is increased 4- to 5-fold if the relative's cancer was found before menopause (the end of menstruation) and involved both breasts. The risk also is increased if breast cancer occurs in several family generations.
About 5% to 10% of all breast cancers are hereditary. Scientists have identified certain genetic mutations (permanent changes in genetic material) that place people at increased risk of breast cancer. To date, the genes that have been most studied include BRCA1 and BRCA2.

Breast cancer risk is increased in women with the longest known exposures to sex hormones, particularly estrogen (female sex hormone). Therefore, breast cancer risk is increased in women who have a history of :-
early first menstrual period (before age 12), late menopause (end of menstruation), no pregnancies, late pregnancy (after age 30), or use of birth control pills (the 'Pill;' oral contraceptives - 'OCs').
It should be mentioned that the Pill's exact hazards are difficult to assess, since risk apparently disappears in women who have not used oral contraceptives for more than 10 years.
Estrogen replacement therapy (ERT), also known as hormone replacement therapy (HRT), is used by many older women to relieve the symptoms of menopause. Certain studies indicate that ERT may increase the risk of breast cancer after long-term use (10+ years). Yet there is no official consensus on ERT, because scientists also have found that the increase in breast cancer risk is eliminated within 5 years of stopping ERT. In addition, some researchers have reported an increased risk of breast cancer in women taking estrogen or estrogen plus progestin, whereas others have not. Because of these uncertainties - and the fact that ERT has a number of positive benefits (e.g., lowered risks of bone fractures and heart attack) - a physician should be consulted about risks and benefits before a person uses ERT.
Most women over-estimate their risk of having breast cancer. If your aunt or grandmother had breast cancer in their 70's, your added risk of getting breast cancer is negligible. The important risk factors are associated with first degree relatives (mother, sister, daughter) especially if they had early onset breast cancer (i.e. breast cancer under 50 years, bilateral breast cancer, or a family history of ovarian cancer). We suggest that women who are under 40 years when diagnosed, or have a strong family history of breast or ovarian cancer see one of our genetic counselors.
If you have had cancer in one breast you have an increased risk of developing cancer in the other breast. This risk can be reduced with drugs like tamoxifen, but the bottom line is that women who have had cancer in one breast should be followed very closely so that if a cancer develops in the other breast it can be caught early.
Most breast biopsies are benign, and do not influence future risk for breast cancer. However, if a woman had a previous biopsy that showed either atypical changes or lobular carcinoma in situ, her risk for breast cancer is increased. These women should seek the guidance of a physician knowledgeable in diseases of the breast. Many of these women would benefit from risk reduction medication such as tamoxifen. They also require careful long-term follow-up.
Prolonged exposure to the combination of estrogen combined with progesterone increases the risk of developing breast cancer. The risk associated with prolonged use of estrogen alone has yet to be defined, but probably will prove to be less than that for combined therapy. Short term replacement therapy for the treatment of menopausal symptoms seems safe. Women who can get by without replacement therapy should do so, but don't forget to have your bone density checked. Women who choose to take replacement therapy for control of symptoms should try to get by on the lowest dose of estrogen for the shortest period of time.


First you stand erect in front of a mirror and check both the breasts for anything unusual - asymmetry, dimpling, puckering, discharge from nipple.


Raise both of your arms.


Now you start examining lower-inner 1/4th portion in the same way. Here you can feel a hard cord of tissue, but do not worry, it is very natural.


Now put your left arm down and start examining below your armpit with your fingers.


Now gently examine your breast from upper outer 1/4 portion towards the armpit.


Lastly examine your breast from the lower inner portion towards nipple.


Lie flat on your bed and check your right breast with left arm and left breast with right arm. If you start from your left breast, then put a towel, or a cloth, or a pillow under you left shoulder and put your left hand behind your head. Use four fingers of your right hand to begin touching your left breast gently and in a circular manner. Examine from upper-inner 1/4 th portion of the left breast to the nipple and examine all the sides of the nipple in the same manner.


Now, put your right hand behind your head and put a thick towel under your right shoulder. Now, start examining your right breast with your left fingers in the same manner.
For most women, breast conservation will be the treatment of choice since it is less traumatic, and the survival results are identical to survival rates with mastectomy. However, not all women are candidates for breast conservation, and some women prefer mastectomy.
Women considering breast conservation must have a clear understanding of the issue of ' margins". The goal in breast conservation is to remove the tumor with a surrounding rim of normal tissue. Obtaining a clear margin can be a challenge. Although the surgeon attempts to take out the entire tumor at the time of the initial surgery, in some cases the tumor cells, which are not visible during the surgery, are found to extend to the edge (margin) of the lumpectomy specimen, and a second operation is required. Fortunately, the vast majority of women who initially choose breast conservation will ultimately achieve a good to excellent cosmetic result. Long-term survival is equal to that with mastectomy.
Some women are either not candidates for breast conservation or choose mastectomy for personal reasons.
Giving chemotherapy first (neoadjuvant therapy) is becoming a more common option. In the past, chemotherapy was given before surgery in situations where the tumor was too large to permit a mastectomy. The chemotherapy was given first to shrink the tumor so that a mastectomy could be successfully performed. It is now becoming common practice to give chemotherapy first to shrink the tumors so that less tissue is taken at the time of the lumpectomy, which leads to improved cosmetic results. We have had extensive experience with this approach and have now saved hundreds of breasts that in the past would have required a mastectomy.
A 6-8 week course of irradiation therapy will be recommended for women undergoing lumpectomy (radiation therapy may be safely avoided in selected women with small, non-invasive cancers). The purpose of radiation is to eliminate any remaining cancer cells in the breast following lumpectomy, and it is very effective in lowering the rate of cancer recurrence in the breast.There is now an alternative to standard radiation therapy which can be accomplished in 5 days .
Radiation is painless and takes only a few minutes to perform. It is much like a simple chest x-ray in that a beam of energy goes through the body without the patient being aware that anything is happening. With breast irradiation the energy beam is much stronger then the energy for a chest x-ray. The most common side effect of breast irradiation is redness to the skin. There is no hair loss or nausea with breast irradiation as there is with chemotherapy.
Lymph node removal will be recommended for most women with breast cancer. Lymph nodes are lima bean shaped structures that vary in size from that of a pea to the size of a marble. A primary function of a lymph node is to filter unwanted materials from the body, and this includes cancer cells. In fact, if breast cancer cells break off from the main tumor, the first place they are likely to go to the lymph nodes under the arm . One of the most important indicators of prognosis is the status of the axillary lymph nodes (i.e. no nodes involved means good prognosis; the more nodes involved, the worse the prognosis). For this reason it was standard therapy in the past to remove all of the lymph nodes under the arm at the time of the removal of the breast cancer to determine prognosis.
It is now standard practice to remove only the first draining lymph node (sentinel lymph node) at this time of the lumpectomy or mastectomy, and have it examined under the microscope. If the lymph node is free of cancer cells , no other lymph nodes are removed. By limiting the number of nodes removed, recovery is accelerated and risk of complications such as lymphedema are minimized.
One of the first questions a woman asks after learning she has breast cancer is: " Am I going to live?" , in other words, " what is my prognosis?" When a woman asks her physician this basic question, she is often frustrated with the vagueness of the response. The problem is that the treating physician does not have enough information following the initial biopsy to make an accurate prediction of survival. Until the tumor and lymph nodes have been removed and analyzed, an accurate prediction of survival is not possible. The most important predictors of survival are the size of the invasive component of the tumor and the status of the regional lymph nodes (when there is no invasive tumor, i.e. only DCIS, the survival rate is 100%). When the invasive tumor is less than 11 mm in diameter and the nodes are negative, the 10 year survival approaches 95%, and if you make it ten years, consider yourself cured. As the tumor enlarges and the number of involved lymph nodes increases, the potential for cure is reduced. However, dramatic improvements have been made in medical treatment of breast cancer (i.e. chemotherapy and hormone therapy) and many new treatments are on the horizon. There is now reason for optimism in even the most advanced cases.
This stage is used to describe non-invasive breast cancer. There is no evidence of cancer cells breaking through to or invading neighboring normal tissue
This stage describes invasive breast cancer (cancer cells are breaking through to or invading neighboring normal tissue) in which
This stage describes invasive breast cancer in which :
Stage III is divided into subcategories known as IIIA and IIIB.
This stage describes invasive breast cancer in which:
The tumor measures larger than five centimeters, OR
The tumor has spread to lymph nodes, and nodes are clumping or sticking to one another or surrounding tissue.
This stage describes invasive breast cancer in which a tumor of any size has spread to the breast skin, chest wall, or internal mammary lymph nodes (located beneath the breast inside the chest)—and includes inflammatory breast cancer.
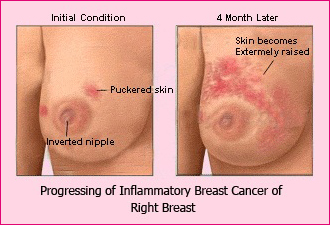
Inflammatory breast cancer is a very common here and very serious, aggressive type of breast cancer that is considered stage IIIB. The most distinguishing feature of inflammatory breast cancer is redness involving part or all of the breast. The redness feels warm. You may see puffiness of the breast's skin that looks like the peel of a navel orange ("peau d'orange"), or even ridges, welts, or hives. And part or all of the breast may be enlarged and hard. Inflammatory breast cancer is sometimes misdiagnosed as a simple infection.
This stage includes invasive breast cancer in which a tumor has spread beyond the breast, underarm, and internal mammary lymph nodes. The tumor may have spread to the supraclavicular lymph nodes (nodes located at the base of the neck, above the collarbone), lungs, liver, bone, or brain.
You may also hear terms such as "early" or "earlier" stage, "later" or "advanced" stage breast cancer. Although these terms are not medically precise (they may be used differently by different doctors), here is a general idea of how they apply to the official staging system.
To date, most inherited cases of breast cancer have been associated with two genes: BRCA1, which stands for Breast Cancer gene one, and BRCA2, or Breast Cancer gene two.
The function of these genes is to keep breast cells growing normally and to prevent any cancer cell growth. But when these genes contain abnormalities, or mutations, they are associated with an increased breast cancer risk. Abnormal BRCA1 and BRCA2 genes may account for up to 10% of all breast cancers.
Women diagnosed with breast cancer who have an abnormal BRCA1 or BRCA2 gene often have a family history of breast cancer, ovarian cancer, or both. But it's also important to remember that most women with breast cancer have no family history of the disease.
But there's still a lot more to learn about these genes. And other genes probably also play a role in the development of breast cancer, for women both with and without a family history of the disease.
This Declaration was adopted by the All India Cancer Support Conference , Delhi: 25 and 26 Nov. 2000
For the well being of people with cancer (adopted by Hitaishini)
A Surgery is the best initial treatment for breast cancer in most women; however, the condition lobular carcinoma in situ (LCIS) usually does not require surgery. LCIS should be watched carefully, though, since breast cancer may develop over time. In some older individuals, LCIS may be controlled by hormone therapy (tamoxifen) alone.
A Although lumpectomy (removal of the tumor and its margins) - combined with radiation therapy - has gained favor as a treatment for early breast cancer, there are some important instances in which mastectomy is a better option. For example, if the tumor lies directly behind the nipple, it may be difficult for the surgeon to remove without significantly altering the shape of the breast. If this is the case, mastectomy may be a better alternative when followed up by breast reconstruction. In addition, women with small breasts may achieve better cosmetic results with mastectomy followed by breast reconstruction.
A If breast cancer has been diagnosed and surgery is proposed, it certainly is advisable to have the operation sooner rather than later. But breast cancer is rarely a surgical "emergency." So it is better to explore surgical options and get a second opinion before scheduling a procedure. Such leeway will permit you to make a more informed decision about your surgery; such as having breast reconstruction at the time of mastectomy, rather than during a separate operation.
A A lumpectomy is - by definition - an operation in which only the cancerous 'lump' is removed, along with a small border of cancer-free tissue (roughly 3/4 in.) and the nearby lymph nodes. This is the surgery to which you have consented. If you still have any questions about surgery - for example, "What will the surgeon do if more cancer than expected is found during surgery?" - discuss them with your surgeon beforehand to avoid any misunderstandings.
A Many women worry that they will have a "hollow" chest after breast cancer surgery. Fortunately, the operations that are performed these days are not likely to produce that kind of disfigurement. If you have a lumpectomy, you will probably have a small indentation in your breast. If you have a modified radical mastectomy or a simple mastectomy, your chest will be flat on the side where the breast was removed. Depending upon the location of your tumor, the scar on your chest wall may be horizontal or diagonal.
A Radiation therapy for breast cancer does not affect the hair on your head, although some hair loss may occur in the armpit area. Some women develop sunburn-like redness and/or skin peeling in the treatment area, whereas others do not. You may be able to predict what to expect by your personal tolerance of sunlight.
A The medications that are used for chemotherapy mostly affect rapidly dividing cancer cells, but they also can injure normal cells. In particular, the rapidly dividing cells of the hair follicles and the lining of the oral/digestive tract may be damaged, causing hair loss and oral/digestive complaints, respectively. Other side effects - some of which are treatable - include nausea, anemia, repeated infections, bleeding, fatigue, and changes in the menstrual cycle. Side effects usually disappear after chemotherapy has ended.
A Most physicians advise women to wait at least 3 years before trying to get pregnant; however, if you are already pregnant or have special considerations, there may be a different answer to this question. There is no overwhelming evidence that pregnancy causes adverse effects in women with breast cancer. But being pregnant while taking the hormone tamoxifen may interfere with the drug's activity and increase the likelihood that your breast cancer will return. It is especially important to practice birth control when taking tamoxifen, as use of this drug is associated with a slight risk of abnormality in the unborn child.
Because many women have had normal, healthy babies during breast cancer therapy, the final decision about pregnancy remains a personal choice.
A Although a "cure" can't be guaranteed in most cases, the majority of women with breast cancer now can expect to live longer and have a better quality of life. In fact, because of recent advances in breast cancer detection and treatment, many breast cancer survivors live a normal lifespan. Even if breast cancer returns, improved therapies may control the disease for a long time.
